Abstract
Background: Cancer or history of cancer are important risk factors for hospitalized patients to develop venous thromboembolism (VTE), manifesting as deep vein thrombosis (DVT) and/or pulmonary embolism (PE). Patients hospitalized for cancer are thus at risk for VTE. However, several studies show that VTE prophylaxis in these patients is challenging and underutilized, with almost 70% of patients with cancer not receiving any VTE prophylaxis as evaluated by our previous analysis. Therefore, this patient population is at risk of recurrent VTE and re-hospitalization. The clinical and economic burden of VTE-related hospital readmissions among these patients is not well understood in the real-world setting. The goal of this retrospective study was thus to analyze the frequency and associated cost of VTE-related hospital readmissions among patients with cancer in the US.
Methods: Patients hospitalized for acute medical illness, including cancer, based on the primary hospital discharge diagnosis codes were identified from the MarketScan databases between 7/1/2011 and 3/31/2015. Eligible patients were ≥40 years and required to have continuous insurance enrollment in the 6 months prior to initial (index) hospitalizations (baseline period) and in the 6 months after hospital discharge (follow-up period). The study endpoints included the proportion of patients with VTE as either the primary or any position (VTE-related) of discharge diagnosis codes among hospital readmissions during the follow-up period, and the associated costs for VTE-related or primary VTE readmissions.
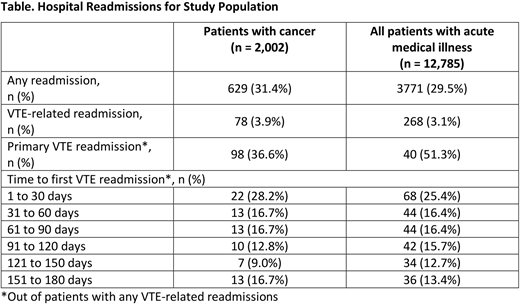
Results: Of the whole study population of acute medically ill patients (n=12,785; mean age: 68.3 years; 51.6% female), 15.7% (n=2,002) were hospitalized for cancer; the mean age was 63.4 years (62% were <65 years) and 49.1% were female. Among patients with cancer, 3.9% had a VTE-related hospital readmission in the 6 months following hospital discharge, of which 51.3% were for a primary diagnosis of VTE (Table). The frequency of readmissions for patients with cancer were the highest among all medical illnesses investigated in this study (acute heart failure, infectious diseases, ischemic stroke, respiratory diseases, and rheumatic diseases). Over one-quarter (28.2%) of the VTE-related hospital readmissions occurred within the first 30 days of post-discharge (Table). For VTE-related readmissions, the mean length of hospital stay (LOS) was 7.6 days and the mean total cost for a hospital readmission was $35,012. For primary VTE readmissions, the mean LOS was 5.2 days and the mean total cost of a readmission was $19,961; for readmissions with a primary diagnosis of DVT, PE, and DVT/PE, mean total costs were $12,968, $13,029, and $41,574, respectively.
Conclusions: In this real-world study, many patients hospitalized for cancer experienced a VTE event requiring re-hospitalization, which was the highest proportion of readmitted patients among acute medical illnesses analyzed in this study, with almost 30% readmitted within 30 days of post-discharge. Total costs of readmissions were substantial, as high as $41K for resubmissions due to primary diagnosis of DVT/PE. Improvement in VTE prophylaxis for patients with cancer may reduce the risk and frequency of VTE, and thus hospital readmissions, reducing the clinical and economic burden of VTE in this patient population.
Sponsorship: Portola Pharmaceuticals
Amin:UC Irvine: Employment; Portola: Consultancy; BMS: Consultancy; Pfizer: Consultancy. Deitelzweig:Ochsner Health System: Employment; Portola: Consultancy, Research Funding, Speakers Bureau; BMS: Consultancy, Research Funding, Speakers Bureau; Pfizer: Consultancy, Speakers Bureau; Boeringer Ingelheim: Consultancy. Lin:Bristol-Myers Squibb: Consultancy; Novosys Health: Employment. Lingohr-Smith:Novosys Health: Employment. Menges:Novosys Health: Employment. Neuman:Portola Pharmaceuticals: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal